Texas Has Stopped Kicking Thousands of Kids Off Medicaid Each Month During the Pandemic, but Advocates Point to Delays for New Enrollees
Texas' frequent eligibility checks for kids on Medicaid are on hold during the COVID-19 public health emergency.

For years, some Texas families have been stuck in a persistent cycle. Their kids are covered by Medicaid, until suddenly they’re kicked off. Sometimes parents don’t realize their children have lost coverage until they’re at the doctor’s office and find out they’ll have to pay out of pocket. Maybe they missed the letter from the state, telling them they needed to submit income verification or other information again. Maybe it arrived the same day the renewal forms were due back, or after those forms were due, or maybe it never arrived at all. So having missed the 10-day window to respond, their children were automatically kicked off Medicaid. Then they have to start a new application. Sometimes the children go without coverage for weeks, even months.
While many states have annual eligibility checks, in 2014 Texas moved to checks multiple times per year for kids on Medicaid, what children’s health advocates say is a burdensome and inaccurate system that kicks thousands of kids off coverage each month and contributes to the state having the highest rate of uninsured kids in the U.S. But these checks are now on hold during the COVID-19 pandemic—a change that advocates have been pushing for for years and one they hope will continue beyond this health crisis.
As part of the federal government’s coronavirus response bill passed in mid-March, in order for states to get increased federal Medicaid funds, they must not unenroll anyone from the program during the COVID-19 public health disaster declaration, unless the person moves out of state or asks to terminate coverage. This includes anyone enrolled in Medicaid as of March 18, from pregnant women, who in Texas would normally have their coverage end two months after giving birth, to children who frequently lose coverage because families aren’t able to return their paperwork within the limited window.
Ending these frequent eligibility checks during the pandemic is critical, advocates say, in part to free up agency staff to focus on processing new applications, as Texans lose their jobs and health coverage for their children. But they say new Medicaid applications are still being held up, leaving families in limbo and kids without coverage.
Texas’ health agency was already facing a significant slowdown in processing benefit applications beginning in November, before the pandemic, says Melissa McChesney, a senior policy analyst at the Center for Public Policy Priorities (CPPP) in Austin. In February, just 67 percent of applications were processed in the federally required 45-day period; in March, that rose to 83 percent, still well below Texas’ norm of 95 percent, according to CPPP. Texas’ Health and Human Services Commission (HHSC) did not say what the rate was in April, or what measures were being taken to expedite applications during the pandemic. According to McChesney, agency officials said a few months ago that delays were due to an increase in applications, and a large number of new staff who were being trained—challenges that are exacerbated now, as employees try to learn new COVID-19 guidelines and rule changes, she says. “Coming into March and into this crisis, the state was digging themselves out of a hole in applications,” McChesney says. “And you see a big increase in applications, so there’s concern that they were not able to process applications as fast, they’re already starting behind, and now there’s a wave of new applications coming.”
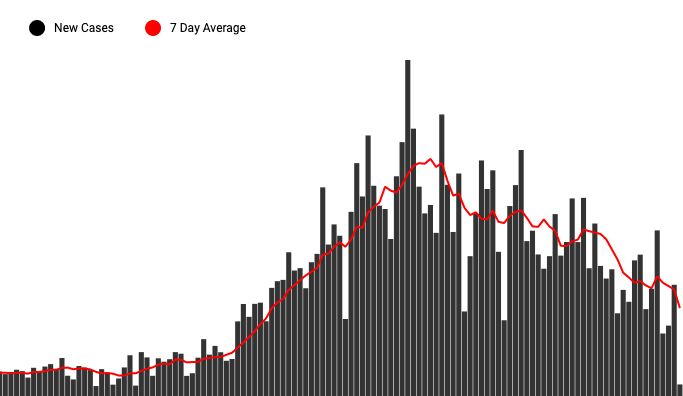
While the renewal checks do appear to have been paused, advocates say that good news comes with several caveats: There is still confusion due to limited communication from the state agency about this change. In some cases, the confusion is driven by renewal letters that went out to families before the March 18 change, requesting income information that’s no longer necessary. Some families are in limbo because kids covered through the Children’s Health Insurance Program (CHIP) have not gotten the same eligibility check suspension. And lags in processing applications for new Medicaid enrollees persist. Particularly given that Medicaid, CHIP, and SNAP are processed through the same agency, advocates fear a continued backlog, as demand for these benefits increases amid skyrocketing unemployment tied to COVID-19.
Graciela Camarena, a program director with the Children’s Defense Fund who works on outreach and enrollment assistance in the Rio Grande Valley, says she’s heard from several families who have waited weeks for word on their Medicaid applications, or been denied, in an apparent error. The pandemic has dramatically reduced an already strained system by making in-person enrollment assistance impossible. People like Camarena are limited in how they can help families sign up for Medicaid from afar, and the state’s phone line for assistance has had persistent hourslong wait times in recent weeks, she says.
Delays and confusion can force families to put Medicaid applications on the back burner as they try to balance more-immediate emergencies. “There’s a combination of things that worry the families that we speak to,” says Camarena. “They’re hurting, their pocketbooks are hurting, their situations have changed, there’s so much uncertainty; is this something they need to make time to do when there are so many other things pressing?” she says. “There are just so many things that families are going through.” So if a letter about their Medicaid application arrives along with an overdue bill saying that their lights will be turned off, Camarena says, “which do you think they’re going to pay attention to?”
Meanwhile, Texas, together with the Trump administration, is continuing to spearhead its lawsuit to eliminate the Affordable Care Act (ACA), potentially stripping health coverage from millions of Americans without any replacement plan. The Supreme Court will hear the case this fall, likely just ahead of the presidential election and as the COVID-19 pandemic continues to unfold. Texas, which has the highest uninsured rate in the country, is one of just 14 states that continue to decline Medicaid expansion under the ACA, which would cover an additional 1.5 million uninsured Texans and help cash-strapped rural hospitals. Without expansion, Texas’ strict eligibility requirements make Medicaid off-limits for most adults, leaving little recourse for those losing their jobs and employer-sponsored coverage.
Advocates and Democratic lawmakers have long pointed to ending frequent income checks and moving to 12-month continuous coverage as the least the state can do to keep eligible kids covered and reduce Texas’ uninsured rate for children. But bills to do so have repeatedly failed. Suspending the checks during the COVID-19 pandemic is an important first step, they say—a kind of test case to hopefully prove the benefits to support a permanent change, if this pause lasts long enough. But it brings uncertainty, too. Families have no way of knowing now when they’ll need to start looking for renewal forms in the mail again, worrying about whether they missed them.
Find all of our coronavirus coverage here.
Read more from the Observer:
-
‘The Pushback’ is an Expansive Look at the Texas Left’s Fight for Power: A new documentary on progressive politics in Texas is an ode to the growing pains of a changing state.
-
COVID-19 Has Infected Workers at a Tyson Beef Plant in Amarillo, Employees Say: The infections are the latest in the surge of coronavirus cases at Texas meatpacking plants and in the Panhandle.
-
Texas Health Officials Undercount COVID-19 Cases by Excluding Some Prisoners Who Tested Positive: The Observer identified at least nine Texas counties where current prison cases make up more than 10 percent of the total COVID-19 cases in the county.